|
Mammography
|
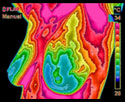
Medical Infrared Imaging
|
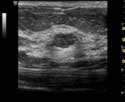
Ultrasound
|
|
|
|
|
| Uses X-rays to produce an image that is a shadow of dense structures. Suspicious areas need to be dense enough to be seen. |
Uses infrared
sensors to detect heat and increased vascularity (angiogenesis) as the
byproduct of biochemical reactions. The heat is compiled into an image
for computerized analysis.
|
High frequency sound waves are bounced off the breast tissue and collected as an echo to produce an image. |
| Structural imaging. Ability to locate the area of suspicious tissue. |
Functional imaging. Detects physiologic changes. Cannot locate the exact area of suspicion inside the breast. |
Structural imaging. Ability to locate the area of suspicious tissue. |
| Early detection method. |
Early detection method. Used as an adjunctive imaging test. |
Low spatial
resolution (cannot see fine detail). Good at distinguishing solid masses
from fluid filled cysts. Used as an adjunctive imaging test. |
Findings increase suspicion.
Cannot diagnose cancer. |
Findings increase suspicion.
Cannot diagnose cancer. |
Findings increase suspicion.
Cannot diagnose cancer. |
|
A biopsy is the only test that can determine if a suspected tissue area is cancerous.
|
| Can detect tumors in the pre-invasive stage. |
May provide the first signal that a problem is developing. |
Ability to detect some cancers missed by mammography. |
|
|
A positive infrared image represents the highest known
risk factor for the existence of or future development of breast cancer –
10 times more significant than any family history of the disease.
|
|
| Average 80%
Sensitivity (20% of cancers missed), in women over age 50. Sensitivity
drops to 60% (40% of cancers missed) in women under age 50. |
Average 90% Sensitivity (10% of cancers missed) in all age groups.
|
Average 83% Sensitivity (17% of cancers missed) in all age groups. |
| Hormone use decreases sensitivity. |
No known effect. |
No known effect. |
| Large, dense, and fibrocystic breasts cause reading difficulties. |
No effect. |
No known effect. |
| In most
women, the medial upper triangle, peripheral areas next to the chest
wall, and the inframammary sulcus cannot be visualized. |
Not applicable.
|
All areas visualized. |
Sources:
Index Medicus – ACS, NEJM, JNCI, J Breast, J Radiology, J Clin Ultrasound
Index Medicus – Cancer, AJOG, Thermology
Text – Atlas of Mammography: New Early Signs in Breast Cancer
Text – Biomedical Thermology
|